Health
6 Early Signs of Prostate Cancer
Prostate cancer is one of the most common types of cancer in males. It starts in the prostate, a small gland about the size of a walnut that is part of the reproductive system. It sits just below the bladder and helps make semen, the fluid that carries sperm.
When cancer grows in the prostate, it usually grows slowly, and many people don’t notice any signs right away. This underlines the importance of knowing signs to watch for. Catching prostate cancer early can make a difference in how it is treated and how well a person recovers.
Urinary Issues
One of the most common early signs of prostate cancer is trouble with urination. Urination is affected because the prostate sits close to the urethra, the tube that carries urine out of the body. If the prostate gets bigger or changes in any way, it can press on the urethra and cause problems.
These urinary symptoms do not always mean cancer. They can be caused by other prostate problems as well, such as an enlarged prostate, also called benign prostatic hypertrophy.
Difficulty Urinating
You may feel the need to urinate but have a hard time getting the stream started. You may also notice that you have to strain to get the urine to come out. Some people feel like they haven’t fully emptied their bladder even immediately after urinating.
Frequent Urination
Needing to urinate more often than usual can be another sign. This urinary frequency can be bothersome as it often occurs at night, while sleeping. Waking up several times a night to use the bathroom could be a sign that your prostate is affecting your bladder.
Weak Urine Stream
Your urine stream might be slower or weaker than normal. It may even stop and start on its own as you attempt to empty your bladder.
Blood in Urine or Semen
Seeing blood in your urine or semen can occur with prostate cancer. Blood may look bright red or brownish in color. Even if you see blood only once, don’t ignore it. Blood can be a sign of prostate cancer or other serious health problems.
Sexual Dysfunction
Some people with prostate cancer may notice changes in their sexual health. One common issue is erectile dysfunction (ED), which is trouble getting or maintaining an erection. Other signs are pain during ejaculation or a decrease in the amount of semen. However, these symptoms might be noticed more after starting treatment for prostate cancer.
Pelvic Pain
Pain in the lower back, hips, or pelvic area might be a sign of prostate cancer. This type of pain usually doesn’t go away and might feel like a dull ache or pressure. It can also cause discomfort when sitting for long periods.
Bone Pain
If prostate cancer metastasizes (spreads outside of the prostate), it will usually spread to the bones. This can cause deep pain in your back, hips, ribs, or legs. The pain may get worse over time or not go away with normal treatment, such as rest or pain medicine. Bone pain can also make it harder to move or walk.
Other Signs: Tests and Screenings
Screening for a disease refers to tests performed on a person with no symptoms of a disease to catch it in its early stages. Guidelines for prostate cancer screening note that people should work with their healthcare provider to consider the benefits of early detection of prostate cancer vs. the risks, such as unnecessary biopsies (removal of tissue to analyze in the lab) and overtreatment.
Men with the following characteristics are considered to be at high risk for prostate cancer:
- Age over 50 years old
- African ancestry
- Having a family member with the disease
- Having a BRCA1 or BRCA2 gene mutation
Prostate-Specific Antigen (PSA) Test
The PSA blood test checks the level of prostate-specific antigen, a protein made by the prostate. This is the first test recommended to screen for prostate cancer. High PSA levels can be a sign of prostate cancer, but they can also mean other prostate issues. If your PSA is high, your healthcare provider may do more tests to determine why.
Digital Rectal Exam (DRE)
The PSA is not the only test that screens for prostate cancer; it is used in combination with a digital rectal exam. In a DRE, a healthcare provider gently inserts a gloved, lubricated finger into the rectum to feel the prostate. They check for lumps, hardness, or changes in size. It might feel a little uncomfortable, but it’s quick and can help detect problems early.
When to See a Healthcare Provider
If you notice any of the warning signs, such as trouble urinating, blood in your urine, or bone pain, contact a healthcare provider. These symptoms don’t always mean that you have cancer, but they should be checked out to be sure. It’s also important to have a discussion with your healthcare provider to learn when prostate cancer screening is appropriate for you.
PEOPLE
Health
Cervical Cancer: Why Vaccination and Screening Can Save Lives

Cervical cancer is a malignant disease that develops in the cervix, the lower portion of the uterus that connects to the vagina. It occurs when abnormal cells in the lining of the cervix begin to grow uncontrollably. Unlike many other cancers, cervical cancer develops slowly, often over many years, progressing from precancerous cellular changes to invasive disease. This long development period makes cervical cancer one of the most preventable and treatable cancers when appropriate screening and preventive measures are in place.
Globally, cervical cancer remains a significant public health concern. It is the fourth most common cancer among women worldwide,after breast, colorectal, and lung cancers. Each year, hundreds of thousands of new cases are diagnosed, and the disease causes a substantial number of cancer-related deaths. The global burden is disproportionately higher in low- and middle-income countries, where limited access to healthcare services, screening programs, and vaccination contributes to late diagnosis and poor outcomes.
The primary cause of cervical cancer is persistent infection with high-risk types of the Human Papillomavirus (HPV), a very common sexually transmitted infection. HPV is a DNA virus which is spread by skin to skin contact. There are over 100 subtypes, most of which do not cause significant disease in humans. Nearly all cases of cervical cancer are linked to HPV, with the majority of diagnoses being linked to HPV types 16 and 18 – to name a few . While most HPV infections resolve on their own without causing harm, long term infection with high risk strains can lead to abnormal cellular changes in the cervix that may progress to cancer if left untreated.
Several factors increase the risk of developing cervical cancer. These include smoking, which weakens the immune system’s ability to clear HPV infections; a weakened immune system due to conditions such as HIV; long-term use of oral contraceptives; early onset of sexual activity; multiple pregnancies; and limited access to regular screening. Socioeconomic factors and lack of awareness also play a role in delayed diagnosis.
In its early stages, cervical cancer often causes no noticeable symptoms, which is why regular screening is crucial. As the disease progresses, symptoms may include abnormal vaginal bleeding (such as bleeding between periods, after sexual intercourse, or after menopause), unusual vaginal discharge, pelvic pain, or pain during intercourse. These symptoms are not exclusive to cervical cancer but should always prompt medical evaluation.
Cervical cancer is highly preventable through a combination of HPV vaccination and regular screening. The HPV vaccine is most effective when administered before exposure to the virus, typically between the ages of 9 and 14. Usually only 2 doses of the vaccine are required at this age, but if over the age of 15, 3 doses are needed. It provides strong protection against the HPV types most likely to cause cervical cancer. Many countries have incorporated the vaccine into their national immunisation programs as a key cancer prevention strategy.
Screening methods such as the Pap smear and HPV testing can detect precancerous changes long before cancer develops. Regular screening allows healthcare providers to treat abnormal cells early, preventing progression to invasive cancer. When cervical cancer is detected at an early stage, treatment success rates are very high. Regular cervical screening decreases the risk of death from cervical cancer by 75%.
Compared to global figures, the incidence of cervical cancer in the United Arab Emirates is relatively low, reflecting the country’s strong healthcare infrastructure and growing emphasis on preventive medicine. However, cervical cancer remains a notable health issue. It is among the top five most common cancers affecting women in the UAE.
Despite the availability of advanced healthcare services, studies and health reports indicate that screening uptake among women in the UAE remains suboptimal. Cultural factors, lack of awareness, fear, and misconceptions about screening procedures can discourage women from undergoing routine Pap smears. As a result, some cases are diagnosed at later stages, when treatment becomes more complex.
The UAE has taken significant steps to reduce the burden of cervical cancer. HPV vaccination was introduced into the national immunisation program in 2018, initially targeting adolescent girls and later expanding to include boys. This reflects a long-term commitment to reducing HPV transmission and protecting future generations.
In addition, national and emirate level health authorities regularly conduct awareness campaigns, particularly during Cervical Cancer Awareness Month, to educate women about risk factors, symptoms, and the importance of screening. Public and private healthcare facilities across the country offer Pap smear and HPV testing services, often at subsidised rates or as part of routine health check-ups.
Conclusion
Cervical cancer is a largely preventable disease with well established methods for early detection and effective treatment. While the global burden remains high, especially in developing regions, countries like the UAE have made notable progress through vaccination, screening programs, and public health initiatives. Continued efforts to increase awareness, improve screening participation, and promote HPV vaccination are essential to further reduce incidence and mortality. With sustained commitment, cervical cancer has the potential to become a rare disease in the UAE, safeguarding the health and well being of women across the nation.
By Dr Dalia Aziz, Consultant Obstetrics & Gynaecologist at NMC Royal Hospital, DIP & NMC Royal Medical Centre, The Palm
Health
Countries With the Most Years in Poor Health
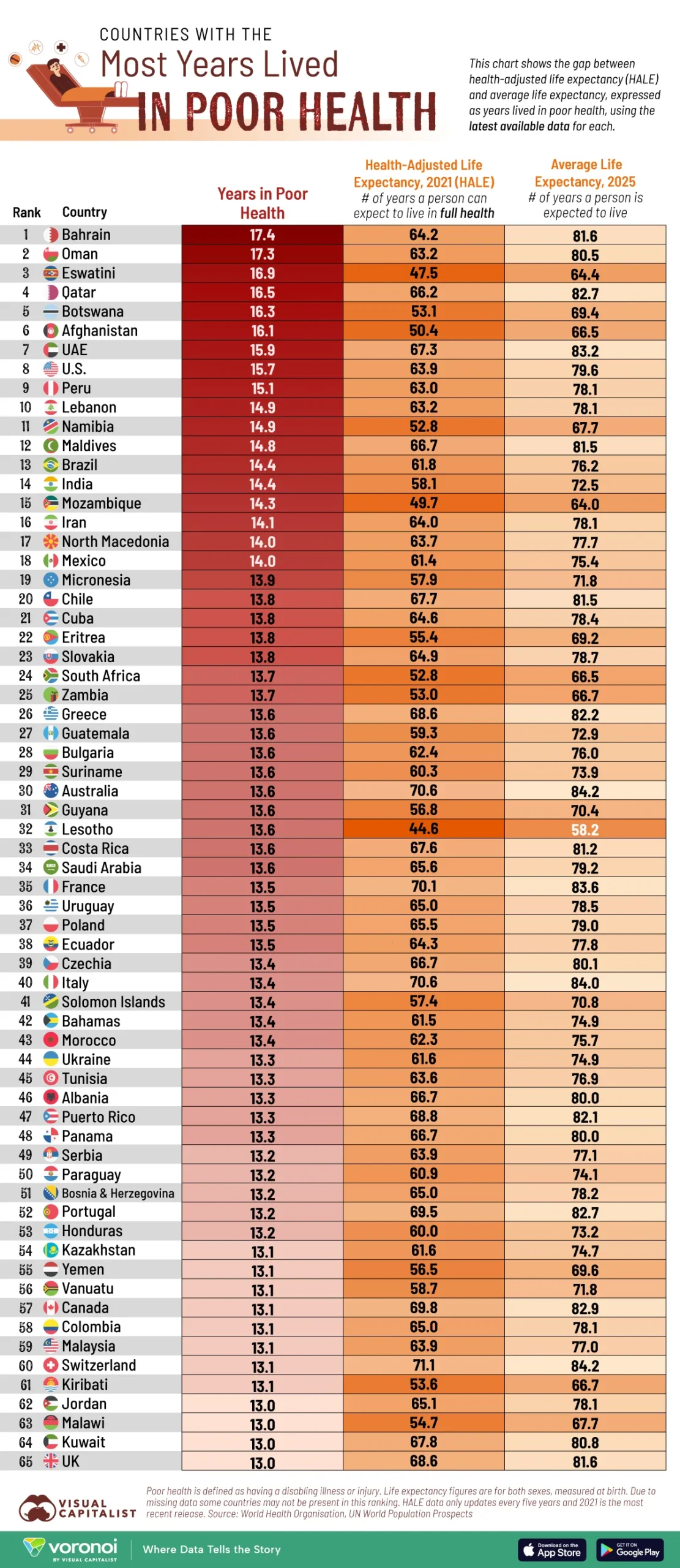
Many people are living longer—but not necessarily healthier—lives.
This visualization ranks countries by the number of years their citizens can expect to live in poor health, calculated as the gap between average life expectancy and health-adjusted life expectancy.
Skip to the second-last section for a full explanation of what health-adjusted life expectancy (HALE) is, and why it matters.
HALE data (for the year 2021) is sourced from the World Bank, via Our World in Data. Average life expectancy is from 2025 estimates UN World Population Prospects.
Together they reveal how disease, disability, and chronic conditions shape the quality—not just the quantity—of our lives.
The Difference Between Living Longer and Living Healthier
Oil wealth appears genuinely toxic to health outcomes.
Nearly every Middle Eastern petrostate (Bahrain, Oman, Qatar, UAE, Kuwait) appears in this worst-performers list.
Bahrain (17.4 years), Oman (17.3), Qatar (16.5), and the UAE (15.9) all post sizable gaps despite having robust health-care budgets.
The lifestyle changes that come with sudden wealth, like sedentary living, processed foods, air conditioning replacing physical activity, seem to create a specific pattern of prolonged morbidity.
The U.S. makes the top 10 as well, the only G7 economy to do. Americans are projected to spend 15.7 of 79.6 expected years in poor health.
Also worth noting is the average life expectancy at birth for all of these aforementioned countries is fairly high. Which means these countries are good at keeping people alive with advanced medical technology.
But they may be failing at keeping them healthy, as if they’ve optimized for extending life rather than living well.
Life Expectancies in Low-Income Countries
s everal sub-Saharan African nations, including Eswatini, Botswana, and Namibia, also record gaps above 14 years.
Unlike the richer Gulf countries, they face this burden alongside much shorter life expectancies, meaning fewer total healthy years.
Latin American countries such as Peru and Brazil post similar gaps, reflecting both higher infant mortalities and higher disease burdens.
These patterns highlight a central challenge for global health: boosting not only how long people live, but how long they live well.
What is HALE (Health-Adjusted Life Expectancy)?
HALE measures how many years a person can expect to live in good health, defined as free from disabling illness or injury.
HALE matters because it fundamentally reframes what we mean by a “successful” life and healthcare system.
Traditional life expectancy tells us how long people live, but HALE tells us how long they live well.
Those “unhealthy years” are extraordinarily expensive. The U.S. healthcare system’s poor HALE performance means they’re essentially running a massive, costly life-support operation for millions of people.
Countries with better HALE ratios spend less on healthcare while achieving better outcomes because they’re preventing problems rather than managing chronic decline.
Source: Ranked
Health
With Exceptional Leadership, Saudi German Health Opens 2026 by Shaping the Future of Healthcare in the UAE

Influential healthcare leadership unites to launch a new year of transformation, collaboration, and human-centred care
Dubai – 16 January 2026
Saudi German Health opened 2026 with a strong statement of leadership by hosting the Multidimensional Community Health Conference in Dubai, reaffirming its role in shaping the future of healthcare across the United Arab Emirates. Held at the Hilton Dubai Palm Jumeirah, the high-level gathering brought together senior decision-makers from regulatory bodies, healthcare operations, and the insurance sector to align on a shared vision for the year ahead.
More than a conventional conference, the event functioned as a strategic forum where leaders moved beyond institutional silos to explore how healthcare delivery can become more integrated, accessible, and personal for patients and families across the UAE.
A Philosophy in Action: Caring Like Family
Rooted in Saudi German Health’s long-standing philosophy, Caring Like Family, discussions throughout the day placed human experience at the centre of healthcare transformation, emphasizing trust, empathy, and continuity of care.
Opening the event, Dr. Ahmed Eissa, Group CEO of Saudi German Health in the UAE, underscored that innovation in healthcare must translate into meaningful outcomes for people.
“At Saudi German Health, we believe that clinical excellence is inseparable from human compassion. This gathering is not just about sharing data or expertise; it is about aligning our efforts to build a healthcare system that is stronger, more transparent, and easier to navigate for every family in the UAE. When we work as one ecosystem, we ensure that the future of medicine remains human at its core.”
Connecting Data, Insurance, and Patient Care
As the UAE advances toward value-based healthcare, the conference examined the evolution of digital health infrastructure, operational efficiency, and modern insurance models that support patient-centred outcomes.
Providing a clinical and operational perspective, Dr. Ahmed Barakat, Hospital Director of Saudi German Hospital Dubai, highlighted how integrated systems directly enhance the patient journey.
“Integrated care is about making complexity invisible to the patient,” said Dr. Barakat. “When data flows seamlessly and teams collaborate across disciplines, efficiency improves—but more importantly, patients experience smoother, safer, and more reassuring care at every stage of their journey.”
Discussions also addressed insurance modernization, emphasizing how data-driven decision-making is strengthening transparency and collaboration between providers and payers.
Setting the Healthcare Roadmap for 2026
With the UAE progressing toward a fully integrated, digitally enabled healthcare model, the conference served as a timely checkpoint for shaping priorities in 2026. Key themes included expanding national digital health platforms to give clinicians a comprehensive view of patient history, optimizing payment and operational systems to reduce fragmentation, and shifting focus toward prevention, wellness, and patient empowerment.
By convening leading healthcare voices at the start of the year, Saudi German Health set a clear direction for the months ahead—one defined by collaboration, innovation, and a deeply human approach to care.
For more information, please visit:
🔗 www.saudigermanhealth.com
-

 Football4 weeks ago
Football4 weeks agoAlgeria, Burkina Faso, Côte d’Ivoire win AFCON 2025 openers
-

 Health1 month ago
Health1 month agoBascom Palmer Eye Institute Abu Dhabi and Emirates Society of Ophthalmology Sign Strategic Partnership Agreement
-

 Health2 weeks ago
Health2 weeks agoNMC Royal Hospital, Khalifa City, performs rare wrist salvage, restoring function for young patient
-

 Football2 months ago
Football2 months agoGlobe Soccer Awards 2025 nominees announced as voting opens in Dubai
-

 Health2 months ago
Health2 months agoEmirates Society of Colorectal Surgery Concludes the 3rd International Congress Under the Leadership of Dr. Sara Al Bastaki
-

 Health2 months ago
Health2 months agoBorn Too Soon: Understanding Premature Birth and the Power of Modern NICU Care
-

 Health4 weeks ago
Health4 weeks agoDecline in Birth Rate in the UAE
-

 Lifestyle2 months ago
Lifestyle2 months agoSaudi Arabia Lifestyle Trends 2025: What You Need to Know About Fitness, Wellness, Healthy Eating & Self-Care Growth



